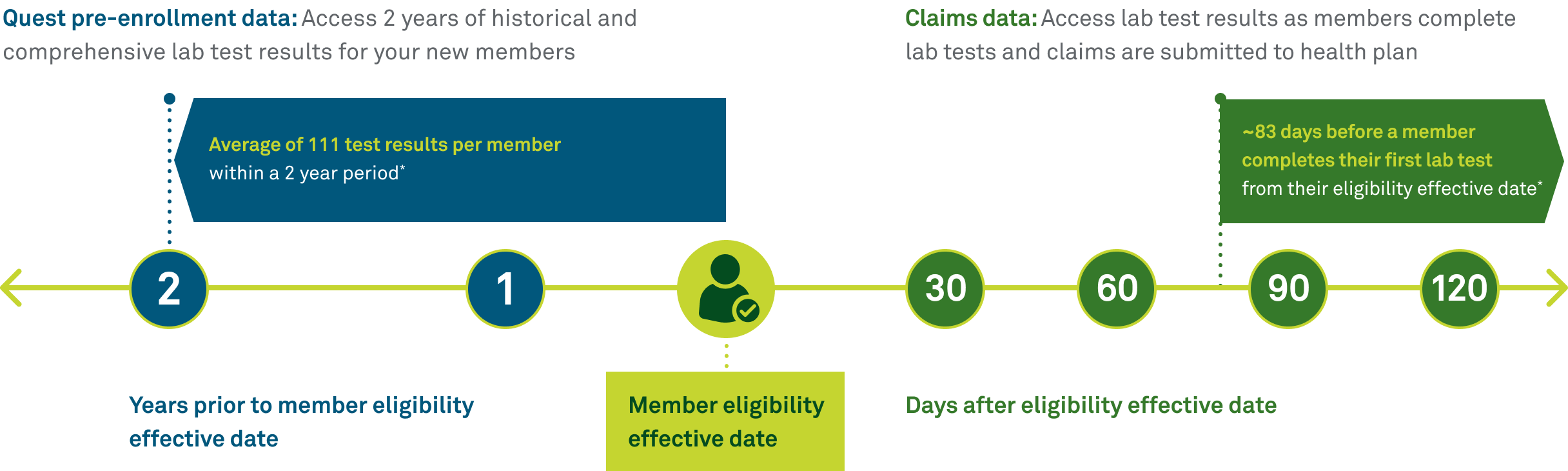
Quest Member Insights pre-enrollment data
Get the latest insights into your new members’ health
Quest Member Insights pre-enrollment data
Get the latest insights into your new members’ health
|
|
Provide insights into disease history and future risk through lab test results |
|
|
Inform disease diagnosis codes (ie, ICD-10) to better reflect hierarchical condition category (HCC) coding and risk adjusted factor (RAF) scores, which may lead to appropriate payments for healthcare coverage |
|
|
Personalize care based on a member’s specific needs; a focus on prevention and early intervention can reduce long-term healthcare costs and improve quality of life |
|
|
Identify and fill in gaps in care for new members to improve HEDIS® measure scores and STAR ratings |
|
|
Deliver better member experiences by understanding your members’ health status and supporting them sooner, potentially leading to higher CAHPS® scores |
Let’s connect
Fill out the form below and a representative will reach out to discuss how our lab data can help your new member initiatives.
|
|
Pre-enrollment data is a part of Quest Member Insights. Click here to learn more. |
Image content features models and is intended for illustrative purposes only.